Stem Cell Dynamics in Neural Tissue Regeneration and Development
Stem cells are vital in developmental neurobiology, playing significant roles in the formation and regeneration of neural tissues. These versatile cells possess the ability to differentiate into various neural cell types, including neurons and glia, which are essential for proper brain function and repair. Their plasticity allows them to adapt to environmental signals, making them prime candidates for therapeutic interventions in neurological disorders. Recent studies have elucidated the molecular and environmental factors that govern stem cell behavior during neural development. Factors such as growth factors, cytokines, and extracellular matrix components influence stem cell fate, proliferation, and survival. Understanding these dynamics is crucial, as it provides insights into how to harness stem cell capabilities for therapeutic regeneration and repair of injured tissues. Therapies utilizing stem cells may transform treatments for conditions like spinal cord injuries, stroke, and neurodegenerative diseases. The multidisciplinary approach combining developmental biology, neuroscience, and regenerative medicine is essential for advancing our knowledge in this field. Future research endeavors will likely refine the techniques used to direct stem cell differentiation, enhancing our ability to promote effective neural tissue regeneration.
The process of neural tissue regeneration governed by stem cells is complex and multifaceted. Following injury or developmental disruption, stem cells respond to signals from damaged areas, initiating repair mechanisms. These signals often recruit surrounding cells, enhancing the regenerative response. In the context of neurodevelopment, stem cells are strategically positioned to generate the diverse cellular populations required for functional neural circuits. Cellular signaling pathways, including Wnt, Notch, and Shh, play crucial roles in maintaining stem cell niches and promoting the appropriate lineage commitment. Research has shown that a well-maintained niche is critical for stem cell health, affecting their proliferation and differentiation capacities. Factors that alter the microenvironment can significantly impact these processes, leading to either successful regeneration or detrimental outcomes. For example, inflammation can alter stem cell behavior, emphasizing the need for understanding the interplay between the immune response and regenerative capacity. Therapeutic strategies may focus on modulating these pathways, utilizing biomaterials, or gene editing technologies. Through such approaches, it’s possible to enhance the efficiency and efficacy of tissue regeneration, paving the way for improved treatments in clinical neurobiology.
Factors Affecting Stem Cell Behavior in the Nervous System
Multiple intrinsic and extrinsic factors influence the behavior and fate of stem cells in the nervous system. One primary intrinsic factor is the genetic makeup of the stem cells, which determines their multipotency and differentiation potential. Understanding the genetic underpinnings can enable scientists to manipulate stem cell populations effectively. Conversely, extrinsic factors include biochemical cues such as growth factors, hormones, and the composition of the extracellular matrix. These cues dictate whether a stem cell will remain quiescent, proliferate, or differentiate into specific neural lineages. Research has focused on how manipulating these external signals can optimize stem cell therapy outcomes. Moreover, age and the overall health of the organism can also influence stem cell function, especially in regenerative contexts. For instance, aged stem cells often show diminished regenerative capacity, highlighting the impact of cellular aging. Innovations in regenerative medicine aim to rejuvenate aged stem cells to restore their functional potential. Overall, understanding the interactions between these various factors is critical for advancing neuroregenerative therapies.
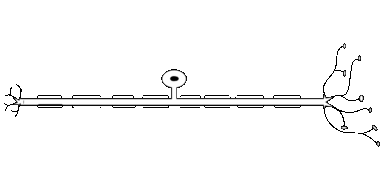
Neural stem cells (NSCs) are characterized by their unique abilities to self-renew and maintain a stable pool of progenitor cells. These NSCs can generate neurons, astrocytes, and oligodendrocytes throughout life, particularly within specific regions of the brain, such as the hippocampus. Such capability is essential for neurogenesis, a process vital for learning and memory. Enhanced understanding of NSC behaviors has broadened options for developing novel therapeutic strategies for neurodegenerative diseases like Alzheimer’s and Parkinson’s. Additionally, the capacity of NSCs to participate in injury response has garnered significant attention for potential treatments following traumatic brain injuries. Researchers are investigating methods to isolate and culture NSCs efficiently, while also deciphering optimal conditions for their expansion. This includes exploring bioreactors that mimic the natural niche where NSCs reside, providing the right mechanical and chemical signals. Furthermore, studies have shown that polarized light and electromagnetic fields can influence NSC activity. This exciting area of research promises innovative approaches for enhancing neural repair mechanisms and ushering in new avenues for treating various brain disorders.
Challenges in Harnessing Stem Cells for Regenerative Medicine
While the promise of stem cell applications in regenerative medicine is immense, considerable challenges remain in the field. One significant obstacle involves the ethical implications surrounding the use of embryonic stem cells, prompting increased interest in alternatives like induced pluripotent stem cells (iPSCs). iPSCs offer the advantage of being patient-specific, thus minimizing immune rejection risks; however, their safety and long-term efficacy remain under investigation. Another challenge involves the inconsistent differentiation of stem cells into desired cell types, which can vary between cell lines and individuals. This variability complicates transplantation strategies and necessitates robust protocols for differentiation. Additionally, issues related to tumorigenicity present a persistent concern when transplanting stem cells into patients. Preventing tumor formation while ensuring adequate tissue regeneration is a critical focus area in ongoing research. Moreover, scaling up stem cell sourcing and maintaining cost-effectiveness for clinical applications pose logistical hurdles. Addressing these challenges requires collaboration among researchers, clinicians, and regulators to develop standardized practices ensuring therapeutic efficacy and safety in stem cell treatments.
Recent advancements in techniques such as CRISPR gene editing have opened new avenues for optimizing stem cell therapies. Through precise gene editing, it is possible to enhance stem cell proliferation and differentiation capabilities, potentially increasing the efficacy of therapeutic approaches for neurodegenerative disorders. Gene editing can also address genetic mutations present in specific diseases, thereby correcting underlying issues at the source. Furthermore, advancements in cell delivery methods, including bioengineering scaffolds or hydrogels, are being explored to improve the integration of transplanted stem cells into existing tissues. The development of novel biomaterials mimicking the natural extracellular matrix can provide a supportive environment, enhancing cell survival and function post-transplantation. Real-time monitoring technologies using bioluminescence or magnetic resonance imaging are also advancing, allowing tracking of transplanted cells in vivo to assess therapeutic efficacy. This integrative approach, combining gene editing with bioengineering strategies, promises to facilitate breakthroughs in regenerating damaged neural tissues. Consequently, ongoing research is expected to produce translational advancements that bring stem cell-based therapies closer to clinical application for treating neurological disorders.
The Future of Neural Tissue Regeneration
The future landscape of neural tissue regeneration holds significant promise as technological advancements continue to emerge. Personalized medicine, integrating patient-specific stem cell lines derived from iPSCs, will likely tailor treatments to individual needs, enhancing treatment success rates. Additionally, interdisciplinary collaborations between biologists, engineers, and clinicians are expected to drive innovative solutions addressing existing challenges in the field. Emphasis on developing reliable protocols for stem cell collection, expansion, and differentiation will further enable researchers to meet clinical and regulatory standards more efficiently. Meanwhile, ongoing research into the cellular microenvironment will illuminate how promoting ideal conditions can enhance stem cell function in both therapeutic and developmental contexts. In parallel, advancements in machine learning and artificial intelligence may facilitate data analysis and parameter optimization in stem cell research, driving efficiencies in experimentation. As these combined efforts unfold, the potential for breakthroughs in treating conditions such as spinal cord injuries, traumatic brain injuries, and neurodegenerative diseases will grow. Collective insights will undoubtedly pave the way for revolutionary therapies, restoring function and enhancing the quality of life for individuals affected by neural injuries.
In conclusion, the dynamic and complex interplay of stem cells within neural tissue regeneration and development underpins advancements in neurobiology and regenerative medicine. These incredible cells hold immense potential for addressing a range of neurological disorders, facilitating repair and restoration of neural structures. As researchers continue to unveil the mechanisms governing stem cell behavior, the prospect of translating this knowledge into effective therapies becomes more tangible. The challenges in harnessing stem cells are significant yet surmountable through collective efforts across disciplines and innovations. Future research focusing on optimizing stem cell applications while navigating ethical considerations, safety, and regulatory concerns holds the promise of elevating patient care in neuroscience. As our understanding deepens, the horizons for stem cell applications in neurodegenerative diseases, injury repair, and brain health are set to expand tremendously. Ultimately, the field of developmental neurobiology will undoubtedly benefit from an increasing appreciation for stem cell dynamics, guiding efforts to rejuvenate and restore neuronal networks. As we look ahead, the excitement surrounding stem cell research continues to grow, inspiring both existing and future generations of scientists to explore this captivating frontier in medicine.