Inflammatory Processes and Their Impact on Brain Development
Inflammation plays a critical role in various biological processes, and its influence on brain development is profound. Neuroinflammation, characterized by the activation of glial cells and the release of pro-inflammatory cytokines, can have significant ramifications during the developmental stages. The central nervous system (CNS) is not immune to inflammation; in fact, early developmental stages are particularly vulnerable. Various factors, including infection, trauma, and environmental toxins, can trigger inflammatory responses that disrupt normal brain development. Recent studies have documented the relationship between maternal infections during pregnancy and the increased risk of neurodevelopmental disorders in offspring. Furthermore, we observe that inflammatory processes not only affect neuronal development but also shape synaptic plasticity and cognitive functions. These alterations in developmental trajectories often have lasting effects on behavior and overall cognitive health. Understanding the role of inflammation is essential, as it can aid in the identification of potential therapeutic targets to mitigate adverse outcomes. Continued research into the underlying mechanisms of inflammation in brain development is necessary for developing effective interventions.
Mechanisms of Inflammatory Responses in Neurodevelopment
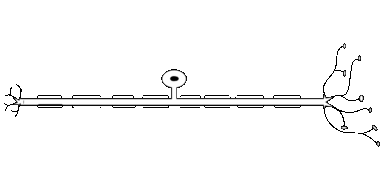
Neurodevelopmental processes involve intricate cellular interactions and signaling pathways that can be dramatically affected by inflammation. During critical periods of brain development, the presence of inflammatory mediators can reshape the architecture of the developing brain. Cytokines, such as TNF-alpha and IL-6, play pivotal roles in modulating neural progenitor cell proliferation and differentiation. When exposure to inflammatory stimuli occurs, it leads to an imbalance in neurotrophic support, potentially resulting in reduced neurogenesis and impaired neuronal survival. Moreover, microglia, the resident immune cells in the CNS, can become activated, leading to the release of neurotoxic substances. This process can hinder the normal growth of axons and dendrites, ultimately compromising synaptic formation and function. Longitudinal studies are crucial for elucidating how these inflammatory events correlate with developmental outcomes. Investigating the timing and severity of inflammation will enhance our understanding of the critical windows during which the brain is most susceptible to damage. This research can pave the way for therapeutic strategies that mitigate the harmful effects of excessive inflammation on neurodevelopment.
The impact of systemic inflammation on the developing brain cannot be overstated. Various prenatal and postnatal factors, including maternal stress and infection, contribute to systemic inflammation that can reach the fetal brain. Maternal immune activation (MIA) during gestation can alter the immune milieu within the womb, leading to altered fetal brain development. Approaches investigating the relationship between early life stressors and inflammatory responses have unveiled compelling evidence linking them to neurodevelopmental outcomes. Infants exposed to high levels of maternal cytokines exhibit cognitive deficits and behavioral issues later in life. Additionally, postnatal exposures to environmental pollutants, such as heavy metals, can initiate chronic inflammatory responses that persist throughout development. Hence, it is crucial to adopt preventive measures to minimize exposure during vulnerability periods. This not only preserves cognitive function but also promotes the healthy development of neural pathways. Future research must focus on pinpointing specific environmental triggers and their mechanisms of action. Understanding how varied environmental factors contribute to systemic inflammation is essential for working towards developing public health strategies aimed at safeguarding brain development.
Neurodevelopmental Disorders Associated with Inflammation
Numerous studies have established a clear link between inflammatory processes and the etiology of neurodevelopmental disorders, including autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD). Children diagnosed with these disorders often exhibit elevated levels of inflammatory markers in their blood, indicating a systemic inflammatory response. The hypothesis suggests that early neuroinflammatory events may disrupt critical periods of brain development, thus influencing the establishment of neural circuits responsible for cognition and behavior. This disruption can manifest as atypical social behavior, communication deficits, and difficulties in attention regulation. Animal models of neurodevelopmental disorders have further corroborated these findings, as manipulated inflammatory processes have led to observable changes in neurobehavioral outcomes. For individuals with an increased genetic predisposition to inflammatory diseases, the risk of developing neurodevelopmental disorders is substantially heightened. Moreover, emerging research seeks to uncover the role of epigenetics in the interaction between inflammation and brain changes over time. Identifying how inflammation catalyzes these disorders can lead to the development of preventative strategies and novel treatment modalities that target inflammatory pathways. Collaborative multidisciplinary research is necessary for further advancement in this area of study.
As awareness of the effects of inflammation on brain development grows, the need for effective interventions becomes apparent. Therapeutic approaches designed to reduce inflammatory responses could potentially alleviate the risks associated with neurodevelopmental disorders. Anti-inflammatory agents are currently being explored as potential treatments to mitigate the effects of inflammation on brain function. However, caution must be exercised when considering medication, particularly in pregnant women, as the safety and efficacy of such treatments remain to be fully understood. Non-pharmacological interventions, such as maternal mental health support and nutritional guidance, could also have a preventive role in minimizing inflammation during critical developmental windows. Furthermore, integrating lifestyle modifications, such as reducing exposure to environmental toxins, may be beneficial. Increasing awareness and providing education about the significance of inflammation can empower parents and caregivers to take proactive steps in creating supportive environments for developing children. It is vital that new research continues to explore the intersection of inflammation, brain health, and cognitive function. By doing so, we can provide valuable resources and solutions to mitigate the negative impact of inflamed states on neurodevelopmental trajectories.
Future Directions in Research
The future of research into inflammation and brain development holds great promise for uncovering novel insights and strategies for intervention. As technology advances, new methodologies, such as single-cell RNA sequencing, are providing unprecedented access to the cellular dynamics of neurodevelopment. This allows researchers to dissect the specific roles of various immune cells in shaping brain structures and functions. Integrating advanced imaging techniques can enhance our understanding of neuroinflammatory processes in real-time, shedding light on how transient inflammatory events influence the developing brain. Moreover, multidisciplinary collaborations combining genetics, neurology, and immunology will be instrumental in addressing the complexities of neurodevelopmental disorders. Large-scale cohort studies will be essential in establishing causative relationships between inflammation and neurodevelopmental outcomes, enabling the development of predictive models. Continued exploration of the gut-brain axis and the role of the microbiome in modulating inflammatory responses will also contribute to our knowledge. Collectively, this research will drive innovations in predictive screening, preventative measures, and therapeutic interventions. Ultimately, understanding these intricate relationships is vital for promoting healthy brain development across populations.
In addition to the scientific exploration of inflammation’s impact on neurodevelopment, public health initiatives should aim to inform communities about the importance of reducing inflammation-related risks. Awareness campaigns can highlight the significance of maternal health and provide resources for screening during pregnancy. Localized interventions that focus on improving maternal diet, reducing stress, and ensuring a supportive environment could serve as proactive measures. Educational efforts in schools can also increase understanding of mental health and behavioral issues associated with neurodevelopmental disorders. By shedding light on the importance of early interventions, these initiatives may help parents recognize symptoms earlier, encouraging them to seek assistance promptly. Collaboration between healthcare professionals, educators, and community organizations creates a synergistic approach to tackling these pressing issues. Policymakers should prioritize funding for research addressing the interplay between environmental factors, inflammatory processes, and brain development. Such public health policies would empower communities to invest in early childhood education and health programs proactively. By mitigating risks associated with neuroinflammation, society can foster healthier developmental outcomes for future generations.
Moreover, interdisciplinary approaches in research are essential for addressing complex biological questions surrounding inflammation and its influence on neurodevelopment. While studies focused on animal models provide critical insights, translation to human development necessitates careful consideration of individual variations. Distinct genetic and environmental factors must be taken into account when evaluating the effects of inflammation on brain growth. The intersection of epigenetic mechanisms offers an exciting avenue for research regarding how environmental triggers interact with genetic predispositions to shape neurodevelopmental outcomes. Longitudinal studies can provide valuable data on how early inflammatory insults impact the brain across different life stages. Such knowledge can inform targeted interventions tailored to specific populations at risk. As evidence accumulates, it will also be increasingly important to seek stakeholder input, including perspectives from individuals with lived experiences of neurodevelopmental disorders. This collaborative approach fosters research that is not only scientifically robust but also socially relevant and meaningful. Building this inclusive research environment will ultimately guide the development of effective programs and policies focused on enhancing brain health across communities.