Placental Physiology and Nutrient Transfer in Mammals
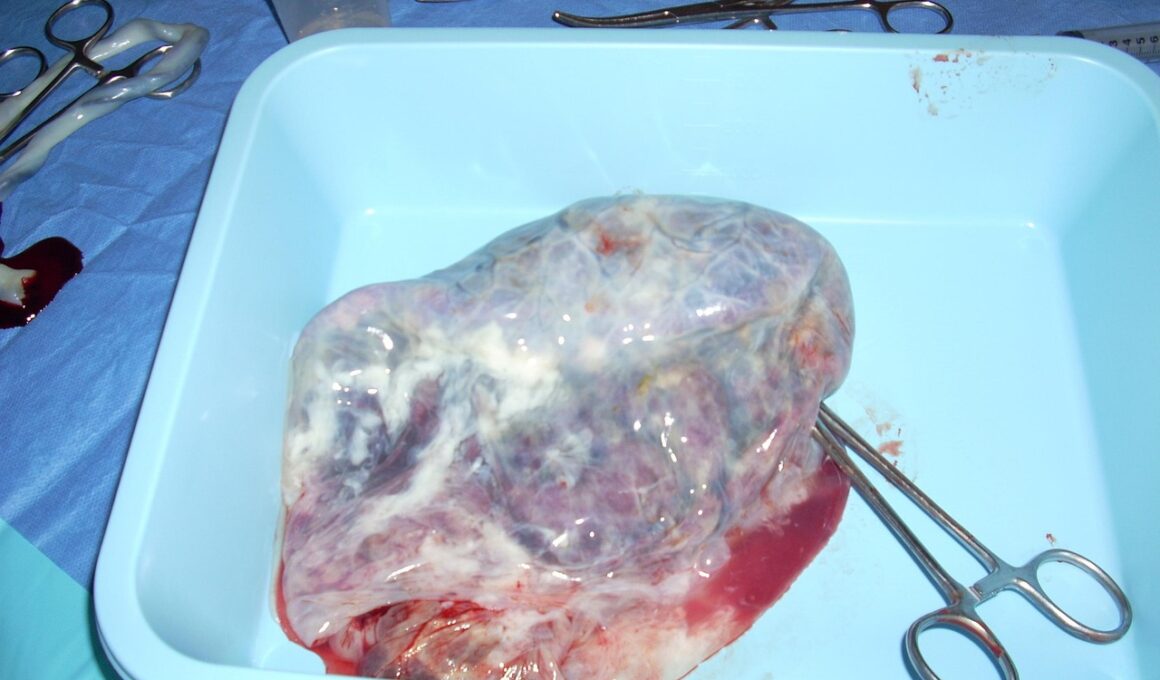
Placental physiology is a critical aspect of mammalian reproduction, as it significantly influences fetal development and health. The placenta serves as a vital organ that facilitates nutrient and gas exchange between the mother and the developing fetus. Understanding the mechanisms of nutrient transfer can aid in deciphering reproductive outcomes in various mammals. The placental interface enables the transfer of essential nutrients such as glucose, amino acids, and lipids while also allowing waste elimination. Different mammals exhibit unique adaptations in placental structure and function, which reflect their specific reproductive strategies. For instance, some species have highly invasive placentas, whereas others possess less-invasive forms. This diversity emphasizes how evolution shapes placental efficiency and adaptability in response to environmental pressures. The role of hormones like human chorionic gonadotropin (hCG) and progesterone in placental function cannot be overstated. These hormones are critical for maintaining pregnancy and ensuring the well-being of the fetus. Research continues to unveil the complexities of placental physiology, and ongoing studies promise new insights into improving maternal and neonatal health outcomes in mammals.
Nutrient transfer mechanisms in the placenta are primarily characterized by diffusion, active transport, and facilitated transport. Each mechanism plays a distinct role in ensuring that the fetus receives adequate nourishment throughout gestation. Diffusion allows the passage of substances along their concentration gradients, making it a primary means for gases like oxygen and carbon dioxide exchange. Conversely, active transport mechanisms utilize energy to move nutrients against their concentration gradients, ensuring the fetus can obtain necessary substances even when maternal supply is low. Transport proteins embedded in the placental membranes facilitate this process, highlighting the complex interactions between maternal and fetal tissues. Furthermore, facilitated transport mechanisms involve specific carrier proteins that assist in moving larger amino acids and sugars across the placental barrier effectively. The interplay between these transport mechanisms influences fetal growth, weight, and overall health. Understanding these processes can aid in identifying potential complications during gestation, such as intrauterine growth restriction (IUGR). Factors influencing nutrient transfer, including maternal health and environmental conditions, also play a crucial role in determining the efficiency of placental nutrient delivery.
Hormonal Regulation of Placental Function
The hormonal regulation of placental function is vital for pregnancy maintenance and successful fetal development. Hormones produced by the placenta and maternal sources significantly influence this dynamic. For instance, human chorionic gonadotropin (hCG) is produced shortly after implantation and plays a pivotal role in stimulating ovarian hormone production. This hormonal support is essential for maintaining pregnancy in the early stages. Progesterone, another key hormone, supports placental development and immune tolerance in the mother’s body. It acts to suppress uterine contractions, facilitating a suitable environment for fetal growth. Additionally, placental lactogen, produced by the placenta, helps regulate maternal metabolism and nutrient mobilization, ensuring that the fetus receives the required sustenance. Research has shown hormonal imbalances can lead to pregnancy complications, such as preeclampsia and gestational diabetes. Understanding the intricate hormonal network is crucial for identifying risks associated with maternal health. Emerging studies suggest targeting hormonal pathways may provide therapeutic avenues to improve pregnancy outcomes. Thus, a comprehensive grasp of hormonal regulation is essential for enhancing both maternal and neonatal health.
The role of the placenta in controlling nutrient transfer extends beyond absorption to include metabolic functions. The placenta actively metabolizes various substrates, which are essential for fetal growth. For instance, it can convert maternal glucose into fatty acids, which are vital for cellular functions and development. Such metabolic activities reflect the placenta’s unique ability to adapt to diverse nutritional environments, which can directly influence neonatal health. Furthermore, the placental barrier regulates the paternal genes that can affect nutrient transfer, impacting offspring characteristics. The differential expression of genes within the placenta also influences how efficiently nutrients are delivered. Importantly, environmental factors such as maternal diet, stress, and age can affect placental function, thus altering fetal nutrient availability. Addressing these factors can help assess prenatal care and potential interventions to optimize fetal development. Research also indicates that inadequate maternal nutrition can predispose offspring to health issues later in life. Therefore, maintaining maternal nutritional status is not only pivotal for immediate fetal health but can also have lasting implications for the offspring’s long-term wellbeing.
Placental Adaptations Across Species
Mammals exhibit remarkable diversity in placental structure and function, which reflects their evolutionary adaptations. Eutherian mammals, or placental mammals, possess complex placentae that provide efficient nutrient transfer, while marsupials have simpler structures. The differences in gestation length and neonatal growth rates significantly correlate with placental morphology. For instance, some eutherians develop a highly invasive placenta that allows for extensive nutrient exchange, promoting rapid fetal growth. In contrast, marsupials give birth at a much earlier developmental stage, leading to prolonged lactation periods and nutrient acquisition from maternal milk. Such adaptations enhance reproductive success in varying environmental contexts. The composition of the placenta also varies, influencing nutrient transport capabilities. For example, the presence of specific transporters can enable the transfer of large molecules essential for fetal development. Understanding these species-specific adaptations can provide insights into evolutionary biology and reproductive strategies. Furthermore, examining endangered and specialized species helps to illuminate how environmental changes impact reproductive physiology. The study of placental adaptations offers promising directions for conservation biology and animal husbandry.
The impact of placental dysfunction on reproductive outcomes is a crucial area of study in reproductive physiology. Conditions such as placental insufficiency can lead to serious complications such as fetal growth restriction (FGR) and stillbirth. These complications arise from impaired nutrient and oxygen supply, which compromises fetal health. Additionally, placental abnormalities can affect hormone secretion, leading to further complications during pregnancy. Addressing these challenges requires a multidisciplinary approach, combining insights from endocrinology, genetics, and maternal-fetal medicine. Early detection of placental dysfunction through advanced imaging techniques can greatly enhance monitoring and management strategies. Furthermore, therapeutic interventions targeting placenta-associated issues show promise in improving maternal and neonatal health. Various studies explore the potential of medications aimed at enhancing placental perfusion or modifying placental function. Nutrition interventions also play a pivotal role in managing placental health. Future research endeavors must focus on understanding the genetic and environmental factors that contribute to placental dysfunction, as this knowledge is essential for developing effective treatments. A comprehensive understanding of placental pathophysiology is fundamental for optimizing pregnancy outcomes and reducing related complications.
Future Directions in Placental Research
The future of placental research holds great potential for enhancing our understanding of reproductive physiology and improving clinical applications. Advanced technologies, such as genomic and proteomic analyses, are paving the way for discovering new biomarkers associated with placental health. These technologies may facilitate early diagnosis of placental-related complications, thus providing timely interventions. Additionally, studies on the microbiome of the placenta have revealed its potential influence on fetal development and immunological outcomes. Understanding the interplay between maternal health, the placental microbiome, and fetal health can lead to innovative treatment approaches. Furthermore, there is a growing interest in investigating artificial placental systems for therapeutic applications. Such models could provide critical insights into nutrient transfer processes and serve as platforms for drug delivery research. The integration of interdisciplinary approaches will likely yield innovative strategies for managing pregnancy-related complications. Greater collaboration among researchers, healthcare professionals, and policymakers will also be crucial for translating findings into clinical practices. Overall, the future directions of placental research offer the promise of substantial advancements in reproductive science and maternal-fetal health outcomes.
In conclusion, understanding placental physiology and nutrient transfer is essential for optimizing mammalian reproductive outcomes. The intricate balance of hormonal regulation, nutrient transport mechanisms, and species-specific adaptations contributes significantly to fetal health. Ongoing research provides valuable insights into the complexities of placental function and its implications for maternal health. By focusing on placental health, targeted interventions can be developed to address complications associated with gestation. Future advancements in research methodologies will provide opportunities to enhance our knowledge and improve clinical applications. The significance of maintaining maternal health is paramount in supporting favorable fetal development and ensuring a successful pregnancy. It is essential for healthcare providers to recognize the importance of placental function in managing pregnancies effectively. Hence, prioritizing maternal nutrition, monitoring placental health, and addressing hormonal imbalances can improve reproductive outcomes significantly. Overall, the multifaceted roles of the placenta underscore its importance in mammalian reproduction, warranting ongoing research efforts to unravel emerging mysteries. As we continue to explore placental physiology, we unlock new possibilities to improve health guidelines and practices surrounding pregnancy.